It's that time of year again. It's the time of year where people say, "Screw it, I'll get back on the wagon after New Years!" This statement is followed by unfettered food consumption and little to no physical activity for 6 weeks followed by a crash diet and Tasmanian Devil levels of physical activity to work off what was put on over the holidays, not to mention the other 5 lbs you gained prior to the binge. What people fail to realize is that their failure was sealed long before they decided to throw caution to the wind and see how many holiday cookies they could eat without getting up on Thanksgiving day.
It's should come as no surprise to anyone that as we get older, our metabolism slows down. What may come as a surprise to most people, if not all, is that research shows that the crash diet you participated in last year probably jeopardized your chance at success this year. Hormones controlling everything from appetite to how much energy you burn take a hit from low calorie dieting, and the negative effect 10 weeks of low calorie dieting has on many of these hormones persists for a year or more(1).
This is one of the many reasons I tell people to stay away from anything like the Isagenix or Medifast programs, short-term results for long-term failure. If you are wondering how I jumped from a low calorie diet to either one of these programs, it's because the low calorie diet in the study above used essentially the same program, Optifast. They all follow the same template, consume 3-5 of our supplements per day, eat little to no food, and watch the fat melt away. What's even more disappointing is that these programs often tout that they are perfectly healthy since they provide 100% of the RDI(Reference daily intake) for micronutrients while also creating a caloric deficit. This may not be the case.
A small study looking at serum and intracellular micronutrient levels in obese people losing weight on the Optifast system paints a starkly different picture. The study followed obese people after following the Optifast 52 plan for 3 months and through 26 weeks of follow-up. It's not surprising that the diet of the participants before the study did not meet the RDI for several micronutrients and many were, therefore, found to have insufficient serum and intracellular levels of multiple micronutrients. What is surprising is that after 3 months of low calorie dieting with shakes that did meet or exceed the RDI of all essential micronutrients, more of the subjects experienced micronutrient deficiencies and some of the micronutrient deficiencies grew worse, particularly Vitamin C, selenium, iron, zinc, and lycopene(2). That doesn't seem very healthy to me.
Some of this can be explained by increased nutrient demand due to weight loss. However, if scientists are a little fuzzy on the micronutrient needs of people participating in a weight loss program, how well read up do you think the person who sold you this product is on the topic? Keep in mind Optifast is only administered by "qualified healthcare providers", which is basically code for someone with an MD who knows nothing about diet. Do you really think the guy at the gym who is schlepping this stuff to you based solely on his personal experience with it has any idea if it's healthy for you?
Interestingly, the participants in the second study who were able to maintain the
fat loss through follow up were able to improve these deficiencies as
they began eating real food. If they were able to maintain the
weight loss eating real food, why not just start there and not risk long
term hormonal dsyregulation due to the low calorie diet? The first
study we looked at showed this altered hormonal state lasts a year and,
unfortunately, follow up in this study only lasted 26 weeks. Who knows
if that weight loss was maintained or not? Maybe this holiday season would be better spent with sane levels of holiday food consumption and high levels of physical activity followed by a nutritious whole food diet at a slight caloric deficit and intelligently programmed exercise?
Thursday, November 20, 2014
Thursday, November 13, 2014
Fibrolmyaglia and Non-celiac Gluten Sensitivity: Two peas in a pod?
Some newer research looking at remission in fibromyalgia recently caught my eye for a few reasons. First, I worked on a clinical trial in fibromyalgia at the University of Pennsylvania a few years back and formed several opinions on what I thought may be predisposing factors to the syndrome. Second, over the course of the last few years I have expanded my knowledge on gut health and gut bacteria to the point where I keep coming back to my thoughts on fibromyalgia and many of the things I thought were potential contributing factors. This new study renewed my interest because it may be shedding light on potential lifestyle modifications that can send fibromyalgia in to remission.
Before I go in depth in to the research, I have to point out that you really cannot make very many hard scientific conclusions based on this information. For one, this data is merely a short communication pinpointing clinical findings of the use of a gluten free diet in people with fibromyalgia. Secondly, this wasn't a random sample of people with fibromyalgia. These people were selected based on certain criteria, specifically that they did not have Celiac disease, they had intraepithelial lymphocytosis, and their symptoms improved on a gluten free diet. While this very specific set of symptoms makes it hard to generalize these results to everyone with fibromyalgia, they honestly make this data far more interesting.
In Fibromyalgia and non-celiac gluten sensitivity: a description with remission of fibromyalgia, physicians in Madrid, Spain chronicle their success at putting patients with fibromyalgia in to remission with a gluten free diet. The study followed 20 patients who met the above criteria for the study and who were willing to try a gluten free diet. The results found all patients had improvement in their pain with 15 of the 20 patients having complete remission of their pain. Fatigue, depression, migraines and GI symptoms all improved with their pain and 2 people with psoriatic arthritis and spondylarthritis, 2 autoimmune conditions, saw remission of those conditions as well.
This data is interesting for a few reasons. First, all but one of the patients had some sort of digestive tract abnormality/issue, and the patient who didn't was the patient who had been diagnosed with fibromyalgia for the shortest period of time(3 years). Indigestion, IBS, constipation, and GERD were the most commonly reported digestive issues. Oral aphthae was also an interesting finding in 2 of the patients. Oral aphthae is essentially recurrent canker sores in the mouth. I've always thought this condition was a barometer of total GI health, and the presence of immune cells in the intestine provide support for this notion.
Next, none of the patients had villous atrophy, a flattening of the villi associated with Celiac disease, but all had intraepithelial lymphocytosis. This isn't a finding because this was part of the inclusion criteria, but it provides significant evidence for the existence of non-celiac gluten sensitivity. Intraepithelial lymphocytosis essentially means something is triggering intestinal inflammation, but it cannot be assumed that gluten is the specific cause just because there is inflammation. Resolution of the problem via a gluten free diet and re-occurence of symptoms in 7 people who reintroduced gluten indicate gluten may be one of, if not the causative factor. The picture below illustrates the stages of progression from normal small intestinal tissue to the damaged villi seen in Celiac disease.
Notice how the normal tissue on the left has projections, called villi, that erode over time in to flat tissue. This is villous atrophy and is caused by intraepithelial lymphocytosis, which is illustrated by the little black dots that slowly infiltrate the intestinal tissue gradually from left to right. As the villi become flattened, a person's ability to absorb nutrients is decreased and they may eventually become deficient in one or more nutrients. In addition, inflammation can dump in to the circulation and cause problems elsewhere in the body. This is where it gets interesting.
For the most part, it has always been assumed that forming antibodies to something called tissue transglutaminase has been the cause of problems outside of the gut due to ingestion of gluten. In Celiac disease, it is believed that tissue transglutaminase binds with gluten and the immune system recognizes this complex as foreign. From there it has been assumed that the immune system mistakes other body tissues as foreign because tissue transglutaminase is found in every cell in the body, but the patients in this study were not forming antibodies to tissue transglutaminase. Therefore, this data does not support the notion that antibodies to tissue transglutaminase is the issue in fibromyalgia, at least not in those who fit the inclusion criteria in this study. So what could be causing the pain?
Interestingly enough, inflammation is known to induce the release of something called nerve growth factor. Nerve growth factor(NGF) has many functions in the body, and in response to inflammation that role is to attempt to reduce it under certain circumstances. NGF is produced locally in tissues but can also be produced by cells of the GI tract and may circulate throughout the body to help maintain homeostasis(1). However, continually assaulting the body with a food that increases inflammation, in this case gluten, will cause more (NGF) to be produced.
Another one of NGFs functions is that it increases pain sensitivity both acutely and chronically in an inflammatory state(2, 3, 4) and administration of anti-NGF drugs reverses this increased sensitivity rapidly(5, 6). Notably, the biggest finding in this short communication is that removal of gluten from the diet of these patients reduced or eliminated their widespread pain. Below is an illustration of the tender points known to be extremely sensitive to touch in people with fibromyalgia.

People with fibromyalgia have an extreme sensitivity to touch in these areas, the slightest brush to the area can cause tremendous pain. In the study I ran, we directly measured the amount of pressure with a dolorimeter and the difference in pain tolerance between someone with fibromyalgia and someone without it is pretty striking. However, these areas tend to be tender for most people indicating that they may have a greater supply of nerve endings than the surrounding tissue. Fascia, a body-wide matrix of connective tissue that runs throughout muscle tissue, is richly innervated with pain receptors. Therefore, it is tempting to hypothesize that the fascia may be involved in the widespread pain associated with fibromyalgia. A recent study found pain receptors in the fascia to be highly prone to the pain sensitizing effects of NGF, and this effect lasted up to 2 weeks(7).
When I worked on the AT101 clinical study on fibromyalgia at UPENN, researchers elsewhere were looking at levels of something called Substance P in the cerebrospinal fluid of people with fibromyalgia as a way to diagnose the syndrome as it is elevated in patients with fibromyalgia. In an interesting twist of fate, Substance P levels in cerebrospinal fluid appear to be associated with cerebrospinal NGF levels and cerebrospinal NGF levels have been shown to be 4x higher in people with primary fibromyalgia than in healthy controls and 2x higher than people with other pain conditions(8).
I have yet to find anything on how blood levels of NGF relate to levels of NGF in cerebrospinal fluid, and NGF appears to play a dual role in inflammation, acting as pro-inflammatory or anti-inflammatory depending on the situation. However, in LPS induced sepsis, NGF appears to have a pro-inflammatory role(9) and this state is similar to what one would experience in non-celiac gluten sensitivity with LPS-containing bacteria from the intestine leaking in to the bloodstream due to a leaky gut. Whether NGF functions as pro- or anti-inflammatory is irrelevant, however, since an increase in NGF that accompanies inflammation likely induces increased sensitivity to pain, the hallmark of fibromyalgia.
I would love to go more in depth with the science aspect in this blog, but it gets pretty dry. The take-home message is that a gluten free diet is a potential therapeutic approach that most people with fibromyalgia likely don't use to their advantage. Even in those who have tried it, the results are variable and can take some time. I've worked with people to eliminate gluten and it's hard enough to get them to go without it for a week, let alone for several months. Another issue is that, for some people, gluten may not trigger intraepithelial lymphocytosis or at least may not be the sole instigator. We are all different and have different sensitivities to food. One of the more important things to consider is not whether or not you should be eating gluten, but whether or not gastrointestinal health should be a central variable in what you consider to be a healthy diet.
In the short communication discussed in this blog, some patients saw quick relief over the course of a few months while others took much longer and the results came along much more slowly. I have a feeling this may have to do with how damaged their GI tract was, how strictly they followed the diet, or whether other foods also triggered a reaction specific to the individual. In addition, other foods such as eggs, coffee, oats, and dairy may have cross-reactivity with gluten, meaning that some of the proteins are similar enough to gluten to give the body the impression that you are eating gluten. Even a small dose of gluten can be problematic for someone who is reacting to it, and a diet containing something the body senses as foreign with a structure similar to gluten may have the same effect as eating gluten itself. For more on gluten cross-reactivity go here. A study looking at a gluten free diet found persistent intraepithelial lymphocytosis in people with Celiac disease despite a long term gluten free diet. The offending nutrient was oats(10), which do not contain the problematic proteins associated with wheat and barley. Cross-contamination may be a potential contributing factor in this study.
Another confounding dietary issue could be the presence of small intestinal bacterial overgrowth, or SIBO. A recent study found that 100% of the people enrolled in the study(42 out of 42) who had fibromyalgia also had SIBO(11). We do not know if this is cause or effect, but eating a reduced FODMAP diet is likely a good idea to help normalize the gastrointestinal flora as SIBO can induce intestinal inflammation. Finally, consumption of foods that contain or cause the release of histamine may be problematic due to the inflammatory effects of histamine. For more information on histamine, check out this blog.
Now, to the bottom line. If you have fibromyalgia, the autoimmune paleo protocol low in FODMAPs and histamine containing and releasing foods is likely the best dietary protocol to help calm down the immune activation in the gut. Below are a couple of links to foods that fit the FODMAP and histamine criteria. After a couple of weeks the hope is that the pain sensitizing effects of NGF will wear off, but it wouldn't surprise me if results took longer. There are other strategies that have to do with exercise, stretching and physical activity that would speed up the process, but we'll save that blog for another day.
A final interesting note on this study. The predominant theory is that once an autoimmune process starts, it will continue throughout life if the environmental trigger is reintroduced. In other words, it would mean lifelong elimination of gluten from the diet. However, this study does not support fibromyalgia as a classic autoimmune disease in that antibodies are not being produced, at least not to tissue transglutaminase. In theory, this means that once the gut is healed, a person may be able to eat gluten in sane quantities provided their gut is healthy and the majority of their diet is centered on maintaining a healthy gut. This would mean that once their gut is healed, it would be beneficial to gradually increase FODMAPs and other types of fiber to promote a more acidic GI tract and to limit inflammation once the SIBO is cleared. However, there is the potential that people with fibromyalgia are forming different antibodies when they ingest gluten, but I don't imagine the science will pick up on that for quite some time.
Histamine in foods
Foods low in FODMAPS
Before I go in depth in to the research, I have to point out that you really cannot make very many hard scientific conclusions based on this information. For one, this data is merely a short communication pinpointing clinical findings of the use of a gluten free diet in people with fibromyalgia. Secondly, this wasn't a random sample of people with fibromyalgia. These people were selected based on certain criteria, specifically that they did not have Celiac disease, they had intraepithelial lymphocytosis, and their symptoms improved on a gluten free diet. While this very specific set of symptoms makes it hard to generalize these results to everyone with fibromyalgia, they honestly make this data far more interesting.
In Fibromyalgia and non-celiac gluten sensitivity: a description with remission of fibromyalgia, physicians in Madrid, Spain chronicle their success at putting patients with fibromyalgia in to remission with a gluten free diet. The study followed 20 patients who met the above criteria for the study and who were willing to try a gluten free diet. The results found all patients had improvement in their pain with 15 of the 20 patients having complete remission of their pain. Fatigue, depression, migraines and GI symptoms all improved with their pain and 2 people with psoriatic arthritis and spondylarthritis, 2 autoimmune conditions, saw remission of those conditions as well.
This data is interesting for a few reasons. First, all but one of the patients had some sort of digestive tract abnormality/issue, and the patient who didn't was the patient who had been diagnosed with fibromyalgia for the shortest period of time(3 years). Indigestion, IBS, constipation, and GERD were the most commonly reported digestive issues. Oral aphthae was also an interesting finding in 2 of the patients. Oral aphthae is essentially recurrent canker sores in the mouth. I've always thought this condition was a barometer of total GI health, and the presence of immune cells in the intestine provide support for this notion.
Next, none of the patients had villous atrophy, a flattening of the villi associated with Celiac disease, but all had intraepithelial lymphocytosis. This isn't a finding because this was part of the inclusion criteria, but it provides significant evidence for the existence of non-celiac gluten sensitivity. Intraepithelial lymphocytosis essentially means something is triggering intestinal inflammation, but it cannot be assumed that gluten is the specific cause just because there is inflammation. Resolution of the problem via a gluten free diet and re-occurence of symptoms in 7 people who reintroduced gluten indicate gluten may be one of, if not the causative factor. The picture below illustrates the stages of progression from normal small intestinal tissue to the damaged villi seen in Celiac disease.
Notice how the normal tissue on the left has projections, called villi, that erode over time in to flat tissue. This is villous atrophy and is caused by intraepithelial lymphocytosis, which is illustrated by the little black dots that slowly infiltrate the intestinal tissue gradually from left to right. As the villi become flattened, a person's ability to absorb nutrients is decreased and they may eventually become deficient in one or more nutrients. In addition, inflammation can dump in to the circulation and cause problems elsewhere in the body. This is where it gets interesting.
For the most part, it has always been assumed that forming antibodies to something called tissue transglutaminase has been the cause of problems outside of the gut due to ingestion of gluten. In Celiac disease, it is believed that tissue transglutaminase binds with gluten and the immune system recognizes this complex as foreign. From there it has been assumed that the immune system mistakes other body tissues as foreign because tissue transglutaminase is found in every cell in the body, but the patients in this study were not forming antibodies to tissue transglutaminase. Therefore, this data does not support the notion that antibodies to tissue transglutaminase is the issue in fibromyalgia, at least not in those who fit the inclusion criteria in this study. So what could be causing the pain?
Interestingly enough, inflammation is known to induce the release of something called nerve growth factor. Nerve growth factor(NGF) has many functions in the body, and in response to inflammation that role is to attempt to reduce it under certain circumstances. NGF is produced locally in tissues but can also be produced by cells of the GI tract and may circulate throughout the body to help maintain homeostasis(1). However, continually assaulting the body with a food that increases inflammation, in this case gluten, will cause more (NGF) to be produced.
Another one of NGFs functions is that it increases pain sensitivity both acutely and chronically in an inflammatory state(2, 3, 4) and administration of anti-NGF drugs reverses this increased sensitivity rapidly(5, 6). Notably, the biggest finding in this short communication is that removal of gluten from the diet of these patients reduced or eliminated their widespread pain. Below is an illustration of the tender points known to be extremely sensitive to touch in people with fibromyalgia.

People with fibromyalgia have an extreme sensitivity to touch in these areas, the slightest brush to the area can cause tremendous pain. In the study I ran, we directly measured the amount of pressure with a dolorimeter and the difference in pain tolerance between someone with fibromyalgia and someone without it is pretty striking. However, these areas tend to be tender for most people indicating that they may have a greater supply of nerve endings than the surrounding tissue. Fascia, a body-wide matrix of connective tissue that runs throughout muscle tissue, is richly innervated with pain receptors. Therefore, it is tempting to hypothesize that the fascia may be involved in the widespread pain associated with fibromyalgia. A recent study found pain receptors in the fascia to be highly prone to the pain sensitizing effects of NGF, and this effect lasted up to 2 weeks(7).
When I worked on the AT101 clinical study on fibromyalgia at UPENN, researchers elsewhere were looking at levels of something called Substance P in the cerebrospinal fluid of people with fibromyalgia as a way to diagnose the syndrome as it is elevated in patients with fibromyalgia. In an interesting twist of fate, Substance P levels in cerebrospinal fluid appear to be associated with cerebrospinal NGF levels and cerebrospinal NGF levels have been shown to be 4x higher in people with primary fibromyalgia than in healthy controls and 2x higher than people with other pain conditions(8).
I have yet to find anything on how blood levels of NGF relate to levels of NGF in cerebrospinal fluid, and NGF appears to play a dual role in inflammation, acting as pro-inflammatory or anti-inflammatory depending on the situation. However, in LPS induced sepsis, NGF appears to have a pro-inflammatory role(9) and this state is similar to what one would experience in non-celiac gluten sensitivity with LPS-containing bacteria from the intestine leaking in to the bloodstream due to a leaky gut. Whether NGF functions as pro- or anti-inflammatory is irrelevant, however, since an increase in NGF that accompanies inflammation likely induces increased sensitivity to pain, the hallmark of fibromyalgia.
I would love to go more in depth with the science aspect in this blog, but it gets pretty dry. The take-home message is that a gluten free diet is a potential therapeutic approach that most people with fibromyalgia likely don't use to their advantage. Even in those who have tried it, the results are variable and can take some time. I've worked with people to eliminate gluten and it's hard enough to get them to go without it for a week, let alone for several months. Another issue is that, for some people, gluten may not trigger intraepithelial lymphocytosis or at least may not be the sole instigator. We are all different and have different sensitivities to food. One of the more important things to consider is not whether or not you should be eating gluten, but whether or not gastrointestinal health should be a central variable in what you consider to be a healthy diet.
In the short communication discussed in this blog, some patients saw quick relief over the course of a few months while others took much longer and the results came along much more slowly. I have a feeling this may have to do with how damaged their GI tract was, how strictly they followed the diet, or whether other foods also triggered a reaction specific to the individual. In addition, other foods such as eggs, coffee, oats, and dairy may have cross-reactivity with gluten, meaning that some of the proteins are similar enough to gluten to give the body the impression that you are eating gluten. Even a small dose of gluten can be problematic for someone who is reacting to it, and a diet containing something the body senses as foreign with a structure similar to gluten may have the same effect as eating gluten itself. For more on gluten cross-reactivity go here. A study looking at a gluten free diet found persistent intraepithelial lymphocytosis in people with Celiac disease despite a long term gluten free diet. The offending nutrient was oats(10), which do not contain the problematic proteins associated with wheat and barley. Cross-contamination may be a potential contributing factor in this study.
Another confounding dietary issue could be the presence of small intestinal bacterial overgrowth, or SIBO. A recent study found that 100% of the people enrolled in the study(42 out of 42) who had fibromyalgia also had SIBO(11). We do not know if this is cause or effect, but eating a reduced FODMAP diet is likely a good idea to help normalize the gastrointestinal flora as SIBO can induce intestinal inflammation. Finally, consumption of foods that contain or cause the release of histamine may be problematic due to the inflammatory effects of histamine. For more information on histamine, check out this blog.
Now, to the bottom line. If you have fibromyalgia, the autoimmune paleo protocol low in FODMAPs and histamine containing and releasing foods is likely the best dietary protocol to help calm down the immune activation in the gut. Below are a couple of links to foods that fit the FODMAP and histamine criteria. After a couple of weeks the hope is that the pain sensitizing effects of NGF will wear off, but it wouldn't surprise me if results took longer. There are other strategies that have to do with exercise, stretching and physical activity that would speed up the process, but we'll save that blog for another day.
A final interesting note on this study. The predominant theory is that once an autoimmune process starts, it will continue throughout life if the environmental trigger is reintroduced. In other words, it would mean lifelong elimination of gluten from the diet. However, this study does not support fibromyalgia as a classic autoimmune disease in that antibodies are not being produced, at least not to tissue transglutaminase. In theory, this means that once the gut is healed, a person may be able to eat gluten in sane quantities provided their gut is healthy and the majority of their diet is centered on maintaining a healthy gut. This would mean that once their gut is healed, it would be beneficial to gradually increase FODMAPs and other types of fiber to promote a more acidic GI tract and to limit inflammation once the SIBO is cleared. However, there is the potential that people with fibromyalgia are forming different antibodies when they ingest gluten, but I don't imagine the science will pick up on that for quite some time.
Histamine in foods
Foods low in FODMAPS
Thursday, November 6, 2014
What the Kale happened to my Iodine?!?!?! Please pass teh almund milkzz!!!!!!
There always seems to be a ginormous pendulum swing every time a food is classified as a "superfood". A relatively obscure food goes from unknown and untouched to eaten 5 times a day with the hope that it will somehow prolong your life or help you lose 15lbs. This pendulum swing is no different when we look at kale. Five years ago no one knew what kale was, now everyone and their mother is eating kale chips, drinking kale smoothies, and eating kale salads at Whole Foods. In some instances, this is not a good thing.
While kale is certainly something that can be part of a healthy diet, we must look at a food from root to tip to determine how big of a part of our diet it should be. There is a lot going for kale from a nutrient standpoint, but there is also a significant drawback, notably that it contains goitrogenic compounds. Goitrogens are substances that can interfere with thyroid function by binding to receptors where iodine should attach. The thyroid turns iodine in to thyroid hormones and a deficiency can lead to thyroid dysfunction. When goitrogens attach to iodine receptors in the thyroid, the thyroid is unable to make thyroid hormones. In theory, if you consume enough goitrogens, you could be getting enough iodine and still be in an iodine deficient state.
I don't believe that this is the typical route that a person consuming kale would be getting themselves in to trouble. In moderation, I don't think kale would have any significant effect on thyroid function. It could interfere with thyroid function when consumed in excess and under the proper conditions, though. First, other cruciferous vegetables such as broccoli, cauliflower, and cabbage also contain goitrogens so you would have to take a look at these other goitrogens in the diet. Second, cooking inactivates some of the goitrogens so people who cook their kale are less likely to have a problem than someone who eats kale smoothies or eats cups of it a day in their salad. Finally, even if you did consume a good amount of kale, it's only likely to become a problem if you aren't taking in sufficient iodine. This is where I think a problem can set in.
Goiter, a swelling of the thyroid due to iodine deficiency was once a significant problem in the United States. It was so big that the landlocked and mountainous areas where goiter was common was referred to as the goiter belt.

To combat this problem, iodine was added to table salt. The result, steep declines of goiter as Americans in the goiter belt were now getting sufficient levels of iodine. I would like to say this is where the story ends, but I don't believe that to be the case. While adding potassium or sodium iodide to table salt helped correct the iodine deficiency, Americans have been turning from table salt to sea salt, which doesn't contain iodine. While I cannot know for sure, I'd imagine this switch is highly prevalent in the kale crowd.
There are other sources of iodine in the American diet. Bread used to have significant amounts of iodine in it until they started using bromine, which happens to also be a goitrogen. Cow dairy also contains significant amounts of iodine. I say this as large swaths of people switch from cow's milk to almond milk while I am still frantically trying to find the teats of an almond. Again, this is a switch I feel is safe to say is quite prevalent in the kale crowd.
So where does this put us with regard to kale? Kale can be a healthy part of your diet provided that the diet is diverse, doesn't focus on kale as an excessive green of choice, and that you get sufficient iodine. Good sources of iodine tend to come from the sea. Kelp and other seaweeds are very good sources as are eggs.
The underlying issue, however, is that people take good foods and call them superfoods to elevate them to the level that they can be consumed endlessly without issue. Kale is a great food, but for someone who is already eating cruciferous vegetables regularly there really isn't any added benefit to eating a lot of kale. It's high in fiber, vitamins A, C and K, and that's about it; these are nutrients that are typically high in vegetables. Kale is also a good source of the omega 3 fatty acid ALA, which would be great except for the fact that humans convert ALA to usable omega-3 fatty acids at less than a 5% rate.
Many boast about the high ORAC score of kale, which is basically a way of measuring how well a food helps the body quash free radicals. Kale is high on the ORAC list...If you don't count berries, about 2 dozen other fruit, pretty much every spice in the world, and at least half a dozen other greens that are freely available at any supermarket such as arugula and beet greens. My point here isn't to prevent you from eating kale, it's to show you that it really isn't appreciably better than most vegetables. So why is it a superfood again?
So where does this put us with regard to kale? Kale can be a healthy part of your diet provided that the diet is diverse, doesn't focus on kale as an excessive green of choice, and that you get sufficient iodine. Good sources of iodine tend to come from the sea. Kelp and other seaweeds are very good sources as are eggs.
The underlying issue, however, is that people take good foods and call them superfoods to elevate them to the level that they can be consumed endlessly without issue. Kale is a great food, but for someone who is already eating cruciferous vegetables regularly there really isn't any added benefit to eating a lot of kale. It's high in fiber, vitamins A, C and K, and that's about it; these are nutrients that are typically high in vegetables. Kale is also a good source of the omega 3 fatty acid ALA, which would be great except for the fact that humans convert ALA to usable omega-3 fatty acids at less than a 5% rate.
Many boast about the high ORAC score of kale, which is basically a way of measuring how well a food helps the body quash free radicals. Kale is high on the ORAC list...If you don't count berries, about 2 dozen other fruit, pretty much every spice in the world, and at least half a dozen other greens that are freely available at any supermarket such as arugula and beet greens. My point here isn't to prevent you from eating kale, it's to show you that it really isn't appreciably better than most vegetables. So why is it a superfood again?
Monday, October 27, 2014
Zucchini pasta with red sauce
Ingredients
2 TBSP olive oil1/4 pound ground beef
2 zucchinis, whole
6 large tomatoes, quartered or chopped
1 yellow bell pepper
1 orange bell pepper
1 1/4 cup yellow onion, diced
1 cup of mushrooms, chopped
6 cloves of garlic, chopped
2/3 oz fresh basil leaves(8 leaves), chopped
2/3 oz fresh oregano, chopped
2 teaspooons of ground black pepper
Salt to taste
Directions
Place cast iron skillet on medium heat and add olive oil. Once heated, add spices and stir. Add onion, peppers, and mushrooms and continue to stir until coated with oil. As the veggies soften, add in the meat and cook until browned. Place tomatoes in a crockpot on low heat and add contents of skillet. Leave on low heat for 6 hours, stir occasionally to break up quartered tomatoes or you can puree in a blender once finished. Once finished, use a vegetti or julienne slicer to make "noodles" out of the zucchini. Serve sauce over zucchini noodles.Nutrition information
Makes 2 servings, each with 6 cups of vegetables513 cals
21g fat
70g carbs
19g fiber
24g protein
3000mg potassium
1236mg sodium (Assuming 1 tsp of salt)
Labels:
Recipes
Monday, October 20, 2014
Asian Hash
Ingredients
1lb of ground turkey sausage2 TBSP of coconut oil
1/2 large onion, diced
12oz bag of Asian slaw or Rainbow salad OR
1/2 cup of broccoli, shredded
1/2 cup of cauliflower, shredded
1/2 cup of carrots
1/2 cup of red cabbage
4 cloves of garlic
1 teaspoon of roasted red pepper
1 teaspoon of black pepper
2 teaspoons of coconut aminos
Directions
Place large cast iron skillet on medium heat and add 1 TBSP of coconut oil and add garlic, roasted red pepper and black pepper, coating with oil. Add sausage and brown. Once sausage is brown, add in other TBSP of coconut oil, Asian slaw, and onions and stir, slowly adding in coconut aminos. Cover for 5-10 mins or until veggies are soft. Salt to taste.Nutrition information
Makes 2 servings519 cals
29g fat
19g carbs
7g fiber
47g protein
1188mg potassium
1451mg sodium
Labels:
Recipes
Thursday, October 16, 2014
Spanish Fries
Ingredients
2 TBSP of bacon grease1/2 large onion, diced
1 large jalapeno pepper, cut in half length-wise and sliced into half discs
2 peeled potatoes, cut with a fry cutter
Garlic powder to taste
Directions
Preheat oven to 425F. Place large cast iron skillet on low heat and add bacon grease. Place cut potatoes in a container with a lid, pour half of grease over fries, add garlic powder, cover, and shake. Place fries on a baking sheet and put in preheated oven. Add onions and peppers to the skillet once its hot and stir. At 10 minutes, shake the fries and put back in for 10 more minutes. When the fires are finished, dump on plate and put onions and peppers on top. Salt to taste.Nutrition information
Makes 2 servings270 cals
13g fat
35g carbs
3g fiber
4g protein
669mg potassium
10mg sodium
Labels:
Recipes
Monday, October 13, 2014
Candida albicans and its effect on hormonal balance
In my previous blog, found here, I went over some of the research on Candida albicans. This opportunistic fungus is the leading cause of fungal infection in humans and can cause issues ranging from mild skin and connective tissue irritation to vaginal yeast infections and hormonal disturbances in those with a candida overgrowth. In this blog I will show the connection behind all 3 of these issues.
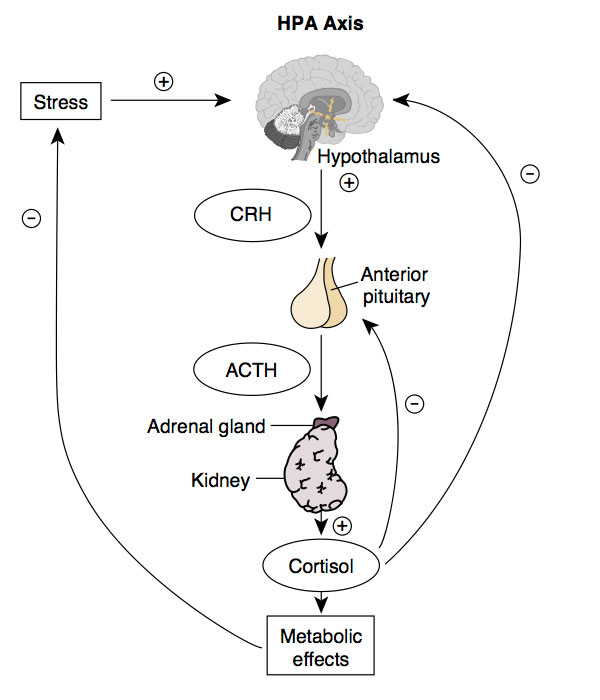
To better understand how Candida albicans can cause a hormonal imbalance, it's important to understand the basic physiology of the stress response. The stress response is carried out by the HPA axis. HPA is an acronym for Hypothalamus-Pituitary-Adrenal.
Recall from my last blog that Candida albicans possesses a corticosteroid receptor capable of binding corticosterone and cortisol. When Candida albicans binds cortisol, it prevents cortisol from binding to cells that need it, while at the same time blocking the negative feedback loop cortisol has on CRH production by the hypothalamus. This can cause the hypothalamus to pump out more and more CRH as it never receives the "Cool it" signal which, in hormonal terms, means the perception of chronic stress. It doesn't end here for the impact on hormonal balance, however. By causing something called pregnenonlone steal, HPA axis mis-signaling due to Candida albicans can cause problems with sex hormones and, therefore, reproductive success.

Pregnenolone is synthesized from cholesterol and becomes whichever steroid the body needs based on hormonal signaling. When cortisol is bound by Candida albicans and the negative feedback loop it has on the HPA axis is broken, CRH sends the signal to the adrenal glands via ACTH that pregnenolone should be converted in to the corticosteroids, particularly cortisol. As pregnenolone is directed towards the corticosteroids, less can be used for formation of sex/reproductive hormones causing a hormonal imbalance. In men, this can cause low testosterone and in women it can cause low testosterone and low levels of estrogens. Estrone, estriol, and estrogen are estrogens and Candida albicans can directly bind estrogen. Ironically, you really don't have to learn anything else to understand how Candida albicans can affect the skin and GI tract because it is by the same mechanism.
By binding corticosterone in the skin, Candida albicans can break the negative feedback loop in the skin's HPA axis which may cause CRH levels in the skin to increase. CRH causes mast cells in the skin to release histamine, an immune compound that increases inflammation and the primary target of antihistamines, pharmaceuticals used to decrease allergic responses(3, 5). Unfettered stimulation of mast cells by CRH could cause skin inflammation to grow out of control and cause major skin hypersensitivity reactions. Increased levels of CRH in the skin are thought to play a role in skin conditions such as eczema, psoriasis, hypersensitivity to chemicals, poison ivy reactions, urticaria, acne, and certain types of hair loss.
It is interesting to note that many of the symptoms of a Candida overgrowth overlap with symptoms of what was once referred to as adrenal fatigue and is now more appropriately labeled HPA axis dysregulation. Another interesting thing that pops up is that many of the symptoms of HPA dsyregulation are caused by an electrolyte imbalance. It is important to note that the adrenal hormone aldosterone is one of the chief regulators of electrolyte balance, and corticosterone is the precursor to aldosterone. Candida could only play a role here if it invaded the adrenal gland directly.
If these mechanisms turn out to be correct, overgrowth of Candida albicans causes HPA axis dysregulation. That is not to say it is the only cause or even the most common cause, other commensal organisms could potentially bind hormones that are part of the HPA axis and could, therefore, cause it to function improperly if they grow out of whack. The important thing to realize if this is the case is that nutrient deficiencies aren't causing the problem, blocking steps in a tightly regulated system is. Therefore, taking high doses of nutrients that are used to manufacture cortisol won't fix the problem until you fix the signaling issue.
***I will likely follow this up with a blog on therapeutic approaches to fixing the problem. However, I need a break from writing these super long, heavily referenced blogs as they take a ton of time and I am currently working on something work related. Please stay patient and hopefully I will get to it soon if that was what you were waiting for. I know, it sucks, but there are only so many hours in the day.
To better understand how Candida albicans can cause a hormonal imbalance, it's important to understand the basic physiology of the stress response. The stress response is carried out by the HPA axis. HPA is an acronym for Hypothalamus-Pituitary-Adrenal.
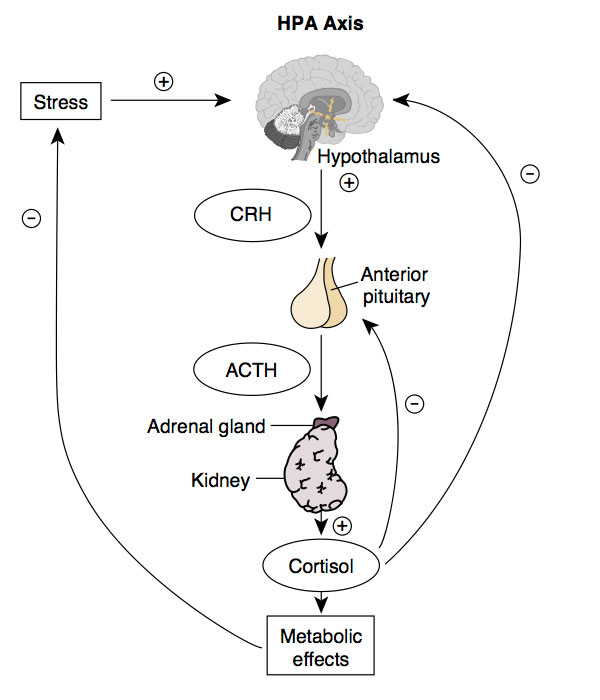
Stress 101
The stress response begins when stress is perceived, which causes the hypothalamus, a part of your brain that is essentially the master control center, to release something called corticotropin releasing hormone(CRH). CRH, in turn, triggers a projection off of your hypothalamus called the the pituitary gland to release adrenocorticotropic hormone (ACTH). ACTH travels in the bloodstream until it reaches an area on top of the kidneys called the adrenal glands and signals them to produce corticosteroids such as cortisol and aldosterone. In turn, as cortisol is pumped out by the adrenals, it eventually makes its way back to the hypothalamus via the bloodstream and shuts off CRH production, which causes the pituitary to reduce production of ACTH which reduces cortisol production by the adrenal glands. This is called a negative feedback loop as higher levels of cortisol help tell the hypothalamus to chill out with requesting more cortisol. While the stress response is far more complicated than this, this is all you need to know to understand Candida albicans' role in causing hormonal disturbances.Recall from my last blog that Candida albicans possesses a corticosteroid receptor capable of binding corticosterone and cortisol. When Candida albicans binds cortisol, it prevents cortisol from binding to cells that need it, while at the same time blocking the negative feedback loop cortisol has on CRH production by the hypothalamus. This can cause the hypothalamus to pump out more and more CRH as it never receives the "Cool it" signal which, in hormonal terms, means the perception of chronic stress. It doesn't end here for the impact on hormonal balance, however. By causing something called pregnenonlone steal, HPA axis mis-signaling due to Candida albicans can cause problems with sex hormones and, therefore, reproductive success.
Pregnenolone-hormonal stem cell
As far as hormones go, pregnenolone is the last common ancestor of all hormones. All steroids begin as pregnenolone and are created based on the body's needs.
Pregnenolone is synthesized from cholesterol and becomes whichever steroid the body needs based on hormonal signaling. When cortisol is bound by Candida albicans and the negative feedback loop it has on the HPA axis is broken, CRH sends the signal to the adrenal glands via ACTH that pregnenolone should be converted in to the corticosteroids, particularly cortisol. As pregnenolone is directed towards the corticosteroids, less can be used for formation of sex/reproductive hormones causing a hormonal imbalance. In men, this can cause low testosterone and in women it can cause low testosterone and low levels of estrogens. Estrone, estriol, and estrogen are estrogens and Candida albicans can directly bind estrogen. Ironically, you really don't have to learn anything else to understand how Candida albicans can affect the skin and GI tract because it is by the same mechanism.
The HPA axis in the skin
In addition to the central HPA axis that regulates the stress response, humans have a peripheral HPA axis within the skin and hair follicles that actively produce the same hormones and contains the same negative feedback system of the central HPA axis(1, 2, 3, 4) with the only difference being that the end product of the skin HPA axis is corticosterone instead of cortisol. The skin and hair follicles are also rich sources of collagen which is high in the amino acid L-Proline, the amino acid of choice for the conversion of yeast to hypha in Candida albicans. When you look at the effect of unmitigated CRH secretion in the skin and GI tract, you can see how Candida albicans can wreak havoc in these tissues.By binding corticosterone in the skin, Candida albicans can break the negative feedback loop in the skin's HPA axis which may cause CRH levels in the skin to increase. CRH causes mast cells in the skin to release histamine, an immune compound that increases inflammation and the primary target of antihistamines, pharmaceuticals used to decrease allergic responses(3, 5). Unfettered stimulation of mast cells by CRH could cause skin inflammation to grow out of control and cause major skin hypersensitivity reactions. Increased levels of CRH in the skin are thought to play a role in skin conditions such as eczema, psoriasis, hypersensitivity to chemicals, poison ivy reactions, urticaria, acne, and certain types of hair loss.
Effects of CRH outside of the skin
High levels of CRH activate mast cells and cause them to release histamine in the intestinal tract, increasing intestinal(6, 7) permeability. CRH is thought to have a major role in IBS(8, 9) which would jibe with the relationship between a exaggerated stress response and IBS. Finally, CRH activates mast cells in the brain and increase permeability of the blood brain barrier(10). An additional effect of chronically high CRH levels in the brain is impaired function of the hippocampus(11), an area of the brain crucial for consolidating information from short-term to long-term memory as well as spatial memory. It is interesting that brain fog is often listed as a potential symptom of candida overgrowth as impaired hippocampal function would certainly be a mechanism for brain fog.Conclusion
Above I have laid out possible mechanisms for the symptoms associated with overgrowth of Candida albicans. It is important to point out that this doesn't mean that if you have one of these symptoms that you have an overgrowth of Candida albicans. If Candida were disrupting signaling within the HPA axis, you wouldn't have a single symptom, you would have a suite of them.It is interesting to note that many of the symptoms of a Candida overgrowth overlap with symptoms of what was once referred to as adrenal fatigue and is now more appropriately labeled HPA axis dysregulation. Another interesting thing that pops up is that many of the symptoms of HPA dsyregulation are caused by an electrolyte imbalance. It is important to note that the adrenal hormone aldosterone is one of the chief regulators of electrolyte balance, and corticosterone is the precursor to aldosterone. Candida could only play a role here if it invaded the adrenal gland directly.
If these mechanisms turn out to be correct, overgrowth of Candida albicans causes HPA axis dysregulation. That is not to say it is the only cause or even the most common cause, other commensal organisms could potentially bind hormones that are part of the HPA axis and could, therefore, cause it to function improperly if they grow out of whack. The important thing to realize if this is the case is that nutrient deficiencies aren't causing the problem, blocking steps in a tightly regulated system is. Therefore, taking high doses of nutrients that are used to manufacture cortisol won't fix the problem until you fix the signaling issue.
***I will likely follow this up with a blog on therapeutic approaches to fixing the problem. However, I need a break from writing these super long, heavily referenced blogs as they take a ton of time and I am currently working on something work related. Please stay patient and hopefully I will get to it soon if that was what you were waiting for. I know, it sucks, but there are only so many hours in the day.
Thursday, October 9, 2014
Candida Albicans: Fact vs Fiction

The internet is filled with tons of information on the fungus Candida albicans. While I love that information is much more accessible now than it has been in the past thanks to the internet, there is a problem with being able to put out and receive any information you like: It's difficult to determine fact from fiction. In this blog I will go over some of the intricacies of Candida albicans and help create a better understanding of what this crazy commensal critter is up to.
What is Candida albicans?
Candida albicans is often referred to as a yeast because overgrowth in the vaginal wall is referred to as a yeast infection, but this is a misnomer. Candida albicans is a fungus that can grow as either single cell yeast or multicelluar filamentous cells. Since it's found in 80% of the human population(1) and more often than not causes no harm to us, it's considered a commensal organism. Candida albicans can convert back and forth between both yeast and hypha depending on the environment it's in, thus it is highly adaptable. The yeast form of Candida albicans is typically benign, it's the filamentous cells that more often than not tend to become problematic, but conversion to filamentous hypha doesn't necessarily have to occur for Candida albicans to cause problems. It is believed that the ability to switch forms and, therefore, adapt to the environment may be the most important factor in the ability of Candida albicans to infect a host rather than just one specific form(2).Since the yeast form is unicellular, it typically spreads out within an environment which causes cells to compete with daughter cells as well as other bacteria found there for real estate and nutrients. Filamentous cells, on the other hand, form hypha that are able to invade host tissues, find nutrients, and help grow biofilms(3). This allows the cells to grow out in to what is more or less a root network, meaning real estate isn't as big of an issue and it can acquire resources in remote areas where other bacteria can't. Even though Candida albicans is considered a commensal organism, it is a frequent cause of infection in patients with a compromised immune system. Below is a picture of Candida albicans in yeast(L) and hyphal(R) form.
Yeast to hypha conversion
While conversion from yeast to filamentous hyphae is not necessary for invasion, this is the most common route due to high expression of the hyphal wall protein-1 gene. When activated, this gene allows the filamentous cells to bind heavily to host tissues, providing stability so that they can form filaments that can puncture and invade host tissues, primarily to scrounge for nutrients. Think of it like outriggers on a drill, without outriggers the drill will topple as it tries to drill in to the ground. When anchored to the ground, stability allows the drill to puncture the ground and the same happens with Candida hyphae. Without adhering to tissue, the hypha would merely push itself away from the tissue rather than puncture through it. Hyphal wall protein-1 is either non-existent or barely expressed in the yeast form of the fungus, but highly expressed in the hyphal form(4).Many people believe high sugar/carbohydrate intake to be the primary culprit in Candida albicans invasion, but the science doesn't support this. In fact, high levels of glucose tend to prevent conversion of yeast to hypha while increased amino acid availability tends to promote it(5). Another factor that tends to promote yeast to hypha conversion is an increased environmental pH, which is promoted through the formation of ammonia when hypha metabolize amino acids. When the yeast form metabolizes glucose, this increases acidity which lowers pH and makes the environment less hospitable to the hyphal form.
If sugar intake is involved at all, it may increase the amount of yeast found within the GI tract. This could indirectly increase the risk of hyphal conversion if the proper conditions present themselves by providing more yeast that could turn in to hyphae, but it doesn't in and of itself promote virulence of Candida albicans under most conditions. Another indirect way sugar intake can promote virulence is through inflammation, which animal models show promotes colonization of Candida albicans(6). This wouldn't be a result of carbohydrate intake, per se, but more likely caused by specific types of food.
Gluten and Candida
When you look at potential dietary issues that may promote Candida albicans invasion, carbohydrate intake does not appear to be directly linked. However, something often found in foods that contain carbohydrate may have a direct effect on Candida albicans yeast to hypha conversion, which increases the likelihood of invasion. Gluten, a protein found in grains, is not completely digested by humans because of it's high content of the amino acids L-Proline and L-Glutamine. This allows gluten to interact with the resident flora within our digestive tract, of which Candida albicans is a member.Studies have shown L-Proline(7, 8) and L-Glutamine(8) to be potent drivers of yeast to hypha conversion, with L-Proline having the biggest effect of any amino acid(9). Candida albicans is also able to bind to free amino acids as well as amino acids that are part of larger proteins(10), as would be the case for a large protein like gluten. Since Candida albicans makes the enzyme needed to break apart proteins high in L-Proline, it could bind to larger proteins and take in L-Proline to induce conversion from yeast to hypha. In addition, gluten is also known to cause inflammation in the GI tract which is another way it may promote the virulence of Candida albicans.
Candida and the immunocompromised
For the most part, the assumption has been that people who are not immunocompromised don't tend to have issues with Candida albicans or other Candida species. However, this is not necessarily true. First, Candida albicans may team up with Streptococcus mutans to form biofilms and cause cavities in the mouths of children(11). Second, a recent study looking post mortem at people who died of heart disease found fungi of the species Candida in plaques from the blood vessel walls during autopsy(12). Another study found significant levels of Candida albicans in the healthy wall of the aorta in patients with coronary artery disease and in the aorta of those with aortic valve stenosis (13). This by no means implies that Candida albicans causes any of these issues, but to say that it is benign in people with a functioning immune system isn't quite true.Up until recently, the model for Candida albicans invasion has required the host to be immunocompromised. However, in 80% of people with disseminated Candida albicans, there is no evidence that they are immunocompromised. In most people, Candida disseminates due to a break down in the permeability of the skin or GI tract or via a change in the gut microbiota. These changes can come about due to surgery, nutrition, and/or antibiotic/antimicrobial usage(14). Even within the GI tract, Candida can become problematic if it overgrows due to its ability to alter hormonal status. This is due to its ability to bind endogenous hormones.
Candida and hormones
Candida albicans can bind female sex hormones, including estrogen(15, 16), and possesses a receptor for corticosteroids that can bind endogenous hormones as effectively as the native corticosteroid receptor(17, 18). Corticosteroids are steroid hormones such as cortisol, corticosterone, and aldosterone that play a significant role in human physiology. Cortisol and corticosterone are glucocorticoids, hormones that prepare the body to deal with stress by increasing blood glucose and suppressing the immune system, among other things. While cortisol is the primary glucocorticoid in humans, corticosterone has a limited role in the human stress response but plays a role in human skin physiology that is just recently being explored. It is also a precursor to aldosterone, a mineralocorticoid that helps regulate electrolyte balance by causing sodium and water to be retained. In addition to binding corticosteroids, the same receptor is capable of binding to progesterone, a precursor to aldosterone and cortisol(19).Conclusion
The ability of Candida albicans to bind to hormones indicates it may have the ability to alter hormonal balance if it overgrows and invades a host. In part 2 of this blog, I will go over how an overgrowth of Candida albicans can cause symptoms ranging from:- HPA axis dysregulation
- Skin sensitivity reactions(Cosmetic sensitivities, hair loss, fungal nail infections)
- Digestive issues
- Hormonal issues
Monday, October 6, 2014
Chicken Kima
Ingredients
1 lb of ground chicken1 large onion, diced
2 medium tomatoes, diced
2 purple sweet potatoes, diced
2 orange sweet potatoes, diced
2 cups of asparagus, cut 2" long
2 TBSP coconut oil
5 cloves of garlic, diced
1 1/4 tsp curry powder
1 tsp of salt, pepper, ground ginger, and turmeric
3/4 tsp of cinnamon
Directions
Place large cast iron skillet on medium heat and add coconut oil. Once the oil is hot, add the onion and garlic and cook until soft and pliable. Add in ground chicken and spices and stir. Once the chicken is browned, add in the tomatoes, asparagus, and sweet potatoes and cook covered until desired firmness, typically no more than 10-15 minutes.Nutrition information
Makes 2 servings511cals
22g fat
52g carbs
11g fiber
33g protein
2115mg potassium
934mg sodium
Labels:
Recipes
Thursday, October 2, 2014
Chicken Tikka Masala (Grain-free, dairy-free)
Paleo Chicken Tikka Masala
Ingredients
4 chicken thighs, pre-roasted and chopped2 tbsp coconut oil
1/8tsp ground ginger
1tsp turmeric
1tsp ground coriander
1tsp cumin
1tsp cayenne powder
1tsp chili powder
dash of cinnamon
5 cloves of garlic, chopped
2 medium vine ripe tomatoes, pureed
1 medium onion, chopped
1 yellow bell pepper, chopped
1 orange bell pepper, chopped
4oz baby bella mushrooms, chopped
1/2 can of lite coconut milk
2tbsp shredded coconut
Salt to taste
Instructions
Place a large cast iron skillet on medium heat and add the coconut oil. Once the oil is melted, add the yellow pepper, onion, garlic, and mushrooms to the skillet and cook until the onions are caramelized. Mix the spices and add to the skillet. Stir the contents of the skillet for a couple of minutes and add the pureed tomatoes, continue to stir. Add the coconut milk and shredded coconut and let simmer for a few minutes. Remove the contents, puree in a blender, and add back to the skillet. Add the chopped chicken thighs and let simmer for 5-10 more minutes.Nutrition information
Makes 2 servings495cals
25g fat
37g carbs
8g fiber
38g protein
1515mg potassium
478mg sodium
Labels:
Recipes
Thursday, September 25, 2014
Movie Review: Fed Up
I think my feelings towards this movie can be summed in 2 words:

While I think the central message given at the end of the movie is a strong one, that people should be primarily eating home-cooked meals made from fresh and local meats and vegetables while limiting or avoiding processed foods, there is too much of what I find to be a recurring theme in most of these movies. This theme is that personal responsibility is not a central part of the answer to our obesity epidemic.
To begin with, there are some parts of this movie that I agree with. The government is certainly making the problem worse by subsidizing bad food, proposing terrible, confusing, and oftentimes conflicting recommendations, and essentially being a puppet for the food industry. Advertising junk food to kids is also a pretty hot button issue that certainly makes a parent's job much more difficult. Finally, bringing the food industry in to school cafeterias is also a pretty troubling move that even the most staunch proponent of liberty would have to question. In the movie they put up clips from the usual bozos from Fox News that decry the nanny state that is reinforced when any form of government regulation on food is proposed. This is a false dichotomy, one can be for personal responsibility/liberty as well as intelligent regulation within the food industry, the problem is intelligence in this country is lacking. If you don't believe this, realize that if you feel that television advertising is damaging to children, you could always turn the TV off. Or, if you still want them to watch television, you could remove the commercials from the program and let them watch their shows a day late.
The movie interviews many children who are dealing with the many health and social complications associated with obesity. You can't help but feel for these children as they tell their stories of being ostracized by classmates and feeling like they are different from their peers. While I believe personal responsibility is going to play a central role in fighting the obesity epidemic, you really can't blame the kids for the problems they face. When dealing with children, I don't believe the lack of personal responsibility lies with them, it lies with their parents. It's not a far cry to say that children that were raised in a household of violence are more likely to raise their kids that way, why is it groundbreaking to think that an adult who is raised to become obese and that becomes obese would raise children that would have the same problem? It's interesting to note that every parent of these children was either very overweight or obese.
This is probably not a popular belief, especially with parents, but it's certainly my belief. While I believe the food advertising directed at kids likely plays a large role in the obesity epidemic, my question is why are the kids spending so much time watching television if the ads are damaging? The answer is simple, it's easy. Likewise, why do parents feed their children processed food or have them purchase lunch in school? Simple, because it's easy. Why don't parents tell their kids no when they ask if they can have cake on a random Tuesday night. The answer, because they know they'll throw a fit. Avoiding a tantrum...is easy. This reminds me of a great stand-up routine by Louis CK. (Warning, NSFW)
Convenience is coveted here in the United States and living a healthy lifestyle is anything but convenient. It's also inconvenient to miss parties with your friends while studying in medical school, but the payoff is certainly worth it. In most instances, delaying instant gratification for long term goal accomplishment tends to be quite satisfying and leads to greater success in the long run. While most parents are fortunate enough to not have to witness the death of their children, is it really any more comforting to know that you're laying down patterns that will likely cause them to die early of something preventable after 5-10 years of suffering that will likely be painful and dramatically impact their quality of life? Go in to a hospital or retirement home and take a look at the patients, each one of those patients was someone's child too.
The movie almost made up for it's shortcomings at the end where it more or less told people the power is with them to make the right choices. However, after spending the whole movie telling people personal responsibility won't cut it and that the government has been screwing everything up, the end essentially promotes personal responsibility and asks for the government to step in. The mom of Brady, one of the kids interviewed for the movie, summed it up best.
"You have to be willing to put forth the effort, it's a matter of priority."
While Brady made tremendous progress when the family followed a diet low in processed food, once he stopped he gained all of the weight back. So when his family prioritized health and put forth the effort to make better decisions, they were able to make incredible health improvements. When they stopped prioritizing and working at it they went back to the way they were. Imagine that.
Overall, I did not like this movie. I believe the message to eat mostly whole, unprocessed food is on target. I believe they dropped the ball on several points. First, exercise was an afterthought and seen as a way to be a scapegoat for the food industry. News flash, exercise is important, that is undeniable. Second, there is universal agreement within the science community that spending time seated in front of a television is one of the worst things for your health. If you reduce the amount of time you sit in front of a television, you will see a lot fewer advertisements and will be much less prone to eat mindlessly, which is another thing with universal consensus as being unhealthy. Finally, I personally believe telling people, particularly children, that they can't do something because the cards are stacked against them is inherently demoralizing. Rather than making them out to be victims of the food industry, how about we raise them to make better decisions and lead by example. Telling a kid they can't do something but then doing it right in front of them really doesn't reinforce the argument that eating bad food is a poor decision, it just reinforces that it's something they will be able to do when they are adults and they will put it on a pedestal. Sort of like drinking alcohol, and we all can see how well telling kids they can't drink until they are 21 has worked to prevent underage drinking.
Monday, September 22, 2014
Endurance exercise, heat tolerance, and gut health
GI disturbances are a frequent complaint in those competing in endurance and ultra-endurance competitions. In addition to GI disturbances, many athletes must cope with heat tolerance issues as well as heat stroke. While many researchers focus on the detrimental effects of endurance exercise on the heart, heat stroke is a much more common occurrence, especially in warmer climates(1). While most endurance athletes probably attribute an intolerance to heat or heat stroke to other mechanisms within the body, the research to date points to immune disturbances caused by increased intestinal permeability as a casuative and/or major contributive factor. In other words, the body's inability to cool down isn't because heat isn't being dissipated properly through sweating, it's because the immune system is being activated. In this blog I will go over the science of what causes this and other factors that can contribute to the problem.
When an endurance athlete competes or performs an intense training run, blood is diverted from the gastrointestinal tract and toward the muscles to power the activity and toward the skin to dissipate heat via sweat. In addition to these changes in circulation, the immune system is also suppressed. This combination of physiological changes, in addition to mechanical jarring of the area, increases intestinal permeability and causes LPS to leak in to the circulation(2, 3, 4, 5). These issues are exacerbated when runs are prolonged, in the heat, and under conditions of dehydration(3). Since LPS drives the immune system nuts, and the immune system is suppressed, it is believed that pushing through causes LPS levels to increase further, and sepsis occurs.
Antibiotic use is known to change the ecology of the gut by modulating gut bacteria. Changes in gut bacteria can lead to alterations in intestinal permeability as many of the byproducts of bacterial fermentation are known to help maintain intestinal barrier integrity. Elimination of a keystone species may impair an athlete's ability to maintain intestinal barrier integrity and lead to greater levels of LPS during exercise and, thus, decreased heat tolerance. This is not to say you shouldn't take antibiotics, but you should only take them when needed and maintain a diet high in fiber when doing so because it will support the bacteria that are responsible for maintaining intestinal barrier integrity.
Certain foods can increase intestinal permeability, particularly ones that contain gluten. Gluten causes the release of zonulin, a protein that causes the tight junctions between cells of the intestine to dissolve. All humans secrete zonulin in response to gluten, but most people reseal the tight junctions rapidly, before significant levels of LPS enter the circulation. People with Celiac disease or a sensitivity to gluten have a delayed response which allows more LPS to enter the circulation and increase inflammation. Researchers believe that this delayed ability to reseal the tight junctions is due to local changes in gut bacteria.
Despite the mass hysteria surrounding gluten, I don't feel that everyone should avoid gluten. In limited quantities in an otherwise vegetable/fiber heavy diet, gluten is likely harmless for most people. However, there is nothing nutritionally novel about gluten that makes it a necessary part of your diet, and most people are likely overeating it while undereating higher quality foods like vegetables.
Chronic alcohol intake is another thing that can increase intestinal permeability and cause damage to the cells of the intestine both directly and as a result of bacterial fermentation(8). The concern here isn't that people are getting loaded before their runs and this impacts their ability to regulate core temperature. The primary concern is that people who chronically ingest alcoholic beverages, particularly beer, may be changing their gut ecology over time in a way that may reduce their ability to reseal tight junctions after distance runs.
Heat as an inducer of heat stroke
The classic model of heat stroke was centered on the notion that once a critical core temperature is reached that is damaging to cells, the hypothalamus decreases the neural drive to muscles. This decreases heat production and, therefore, core temperature. So, in essence, there is a safety mechanism built within the hypothalamus that prevents core temperature from exceeding a certain point that could be detrimental to the cells of the body. While this is true, there are a couple of issues that contradict this model. First, people often experience heat stroke at workloads they have previously tolerated, both in terms of performance and heat stress. Second, core temperature doesn't seem to share a relationship with the severity of symptoms experienced once heat stroke is triggered, but there is a strong relationship between symptom severity and circulating inflammatory cytokines(2).The immune system as an inducer of heat stroke
These factors have caused researchers to propose a dual model of heat stroke that has a heat induced pathway and an immune system induced pathway. There doesn't appear to be a specific core temperature at which heat stroke is induced between individuals or within the same individual, and many of the clinical manifestations of heat stroke are identical to those found in sepsis, a whole body inflammatory response to infection. It is believed that endotoxemia, the leakage of lipopolysaccharide(LPS) from the gut in to the circulation due to increased intestinal permeability, drives this inflammatory process. This has led scientists to develop an endotoxemia model of heat stroke where hyperthermia initiates heat stroke by increasing intestinal permeability, but endotoxemia drives the clinical progression. It is believed that this model of heat stroke is the primary cause as the vast majority of people who experience heat stroke are not reaching the critical core temperature that is damaging to cells(2).When an endurance athlete competes or performs an intense training run, blood is diverted from the gastrointestinal tract and toward the muscles to power the activity and toward the skin to dissipate heat via sweat. In addition to these changes in circulation, the immune system is also suppressed. This combination of physiological changes, in addition to mechanical jarring of the area, increases intestinal permeability and causes LPS to leak in to the circulation(2, 3, 4, 5). These issues are exacerbated when runs are prolonged, in the heat, and under conditions of dehydration(3). Since LPS drives the immune system nuts, and the immune system is suppressed, it is believed that pushing through causes LPS levels to increase further, and sepsis occurs.
The immune system and chronic endurance exercise
This may sound like a whole bunch of doom and gloom for people undertaking endurance exercise, but the body adapts. A chronic adaptation to long term endurance training is an increase in anti-LPS antibodies(2, 4). This means training at or above the threshold that causes LPS to leak from the GI tract in to the circulation causes the body to deal with LPS better. However, this brings up a couple of interesting questions. Why would a well trained, experienced runner experience heat stroke during a run of tolerable intensity? Also, how can some trained athletes tolerate levels of heat that induce heat stroke in others?Internal vs. external environmental conditions
Obviously external environmental conditions, especially in extremely hot environments, could be at play, but what about internal environmental conditions? In other words, maybe it isn't the state of the environment that is causing the problem, maybe it's the physiological state of the athlete. One potential contributing factor is obvious; training during an infection. The trio of an existing infection, an acutely depressed immune system, and LPS leaking from the gut in to the circulation could negatively impact heat tolerance causing once manageable workloads to cause unmanageable levels of LPS. There is data to support the evidence that immune disturbances can lead to transient heat intolerance(2). Furthermore, many animal studies show that heat tolerance is improved and heat stroke can be averted up to a point when animals are given therapies to help deal with LPS. Animals given therapy to bolster LPS clearance are better able to tolerate heat and do not succumb to heat stroke until temperatures exceed 43.8C, which is considered the critical temperature for cell damage(2). In a small study, all monkeys who were given anti-LPS antibodies were able to survive at 43.5C but only 16% of control monkeys lived as the rest succumbed to heat stroke(6). When core temperature was raised to 43.8C, all of the monkeys died but the treated monkeys lived 5 times longer than the controls.Gut health as a contributing factor
Another avenue worth exploring is the health of the gut. Many factors affect intestinal permeability under what would be considered resting conditions including the use of anti-inflammatory drugs, antibiotic use, and diet. A recent study looking at the use of ibuprofen found that intestinal permeability after exercise was greater when an athlete took ibuprofen than when they did not(7). This is important because many athletes use anti-inflammatories as a training tool to help reduce inflammation, and this study shows that there may be drawbacks to using this approach.Antibiotic use is known to change the ecology of the gut by modulating gut bacteria. Changes in gut bacteria can lead to alterations in intestinal permeability as many of the byproducts of bacterial fermentation are known to help maintain intestinal barrier integrity. Elimination of a keystone species may impair an athlete's ability to maintain intestinal barrier integrity and lead to greater levels of LPS during exercise and, thus, decreased heat tolerance. This is not to say you shouldn't take antibiotics, but you should only take them when needed and maintain a diet high in fiber when doing so because it will support the bacteria that are responsible for maintaining intestinal barrier integrity.
Diet as a preventative therapy
This brings us to diet, one of the most important "therapies" a person can use to maintain optimal intestinal barrier integrity. A proper diet helps maintain intestinal barrier integrity by optimizing gut bacteria, providing nutrients that gut bacteria can use to uphold the intestinal barrier, and limiting the types of food that can increase intestinal permeability. Under optimal conditions, the intestinal barrier is maintained by tight junctions, areas between cells that don't allow contents of the intestine, including LPS, in to the bloodstream. These tight junctions can be dissolved under certain conditions, and the fermentation of soluble fiber and resistant starches by resident bacteria generate short-chain fatty acids that reseal these tight junctions.Certain foods can increase intestinal permeability, particularly ones that contain gluten. Gluten causes the release of zonulin, a protein that causes the tight junctions between cells of the intestine to dissolve. All humans secrete zonulin in response to gluten, but most people reseal the tight junctions rapidly, before significant levels of LPS enter the circulation. People with Celiac disease or a sensitivity to gluten have a delayed response which allows more LPS to enter the circulation and increase inflammation. Researchers believe that this delayed ability to reseal the tight junctions is due to local changes in gut bacteria.
Despite the mass hysteria surrounding gluten, I don't feel that everyone should avoid gluten. In limited quantities in an otherwise vegetable/fiber heavy diet, gluten is likely harmless for most people. However, there is nothing nutritionally novel about gluten that makes it a necessary part of your diet, and most people are likely overeating it while undereating higher quality foods like vegetables.
Chronic alcohol intake is another thing that can increase intestinal permeability and cause damage to the cells of the intestine both directly and as a result of bacterial fermentation(8). The concern here isn't that people are getting loaded before their runs and this impacts their ability to regulate core temperature. The primary concern is that people who chronically ingest alcoholic beverages, particularly beer, may be changing their gut ecology over time in a way that may reduce their ability to reseal tight junctions after distance runs.
Conclusion
As research on the topic of gut health progresses, we find more and more physiological processes that gut health affects. This blog presents compelling evidence that gut health can directly impact performance in endurance competitions through modification in heat tolerance. If you take one thing from this blog, it should be that it is in your best interest to pay attention to the quality of your diet. While research on gut bacteria and gut health is in it's infancy, the one common thread in all of the data is that a diverse microbiome is best for gut health, and a diverse diet is what's best for a diverse microbiome. Including as many different fruits and vegetables as possible will help build a diverse microbiome and provide enough fiber to help maintain intestinal barrier integrity as you train throughout the year. In addition, the use of anti-inflammatories should be used with caution and diet quality should be tightened up during an infection that requires the use of antibiotics.
Labels:
Exercise,
Gut health
Thursday, September 18, 2014
No free lunch: No calorie sweeteners shown to cause gut changes that induce glucose intolerance

No-calorie sweeteners have proven to be relatively useless in the fight against obesity, despite what the food industry may tell you. In a new study published in Nature, researchers provide evidence that no-calorie sweeteners can induce metabolic changes that lead to glucose intolerance in both mice and humans. This study found that the changes in glucose tolerance come about from shifts in gut bacteria.
The mouse arm of this study started by feeding mice a 10% solution of either saccharin, aspartame, or sucralose in place of drinking water and comparing their glucose tolerance to control mice given either water alone or a 10% glucose solution. After 11 weeks, the glucose tolerance in the mice given the artificial sweetener was worse than the mice given water or even glucose. Previous research has shown that certain no calorie sweeteners can alter the gut microbiome, so the researchers gave mice a 4 week course of antibiotics to wipe out the microbiome. The result...Glucose tolerance returned to normal.
To make certain that the effects were due strictly to changes in the gut microbiome, researchers transplanted feces from the mice given saccharin in to germ-free mice who had not had the sweetener. Within a week, the germ-free mice had the same changes in glucose tolerance as those who consumed the no-calorie sweetener. Looking at the fecal samples, researchers found changes in the microbiome that mirrored changes in the microbiome of humans that eat no-calorie sweeteners. Furthermore, a follow-up with 7 humans with no history of using no-calorie sweeteners who were fed saccharin at the maximum daily limit allowed by the FDA found that 4 of the subjects had poorer glucose tolerance after 7 days and an altered gut microbiome that, when transplanted in to mice, resembled the one seen in mice fed saccharin.
This study brings up a few important points. While the dosage of no-calorie sweetener was high, it was within FDA limits. So while you may not consume these sweeteners at the level seen in these studies, the point is that they aren't entirely benign. Furthermore, relying on these sweeteners as a crutch to kick a sweet tooth may not be in your best interest, especially if you are diabetic. Secondly, some people did not respond negatively to the no-calorie sweetener. An important question to answer would be whether or not Type 2 diabetics, who have poor glycemic control in the first place, are more likely to be susceptible to poorer glycemic control from these sweeteners due to their microbiome. I would be willing to bet that people with Type 2 diabetes are more likely to rely on no-calorie sweeteners because they "have no direct effect on blood glucose". Unfortunately, they apparently have an indirect effect on blood glucose that is just as bad as a direct one.
Finally, even though the people who weren't affected by the artificial sweeteners were in the minority, the fact that their glucose tolerance wasn't affected, nor was their microbiome, points to no-calorie sweeteners being benign for them. As is a frequent topic in this blog, an individualized approach to health and diet is always the best approach.
Thursday, September 11, 2014
Why Lebron James needs (the right kind of) carbs
http://online.wsj.com/articles/why-lebron-james-is-suddenly-skinny-1408388466
The world is abuzz with Lebron James' recent decision to undertake a low carbohydrate Paleo diet and the more svelte physique that followed. While the aesthetic change to his decision is readily apparent, the performance ramifications wait to be seen. As someone who has used principles of the Paleo diet for my own personal nutrition as well as those of my clients for the past 5 years, I am familiar with the ins and outs of this type of nutrition program. While paying more attention to the quality of one's diet can improve performance, cutting carbohydrates is not always the best idea for someone in a sport like basketball.
The type of fuel a person uses is dependent on the type of activity they partake in. Someone who sits at a desk and does low level physical activity throughout the day doesn't need a large amount of carbohydrate because this type of activity predominantly uses fat. If this person were to get up and sprint on and off for 30 seconds at a time they would shift to burning glucose, which is what the body turns carbohydrates in to. In the event this person decides not to eat carbohydrate and still tries to perform physical activity that requires glucose from carbohydrates, they will eventually "bonk". This means they will not be able to produce energy fast enough to keep up with demand. While they will be able to make glucose from non-carbohydrate energy sources, the body cannot produce it fast enough to keep up with the demands of a sport like basketball. My prediction: Either Lebron starts eating carbohydratess or his game will suffer.
So if slashing carbohydrates isn't going to give a performance advantage, how can following principles of the Paleo diet improve athletic performance? To better understand how this works, it's important to get a basic understanding of how the immune system works. I promise this won't get too technical. Monocytes are essentially immature white blood cells, they roam around the bloodstream like a couple of high schoolers looking for something to do. Just like a high schooler, they have no specialized skill because they haven't received instruction yet. When monocytes encounter an area of the body in need, they quickly receive a PhD in what needs to be done from the environment and differentiate in to a more specialized type of cell that can carry out a more specific task in that tissue. This could be to identify invaders, fight an infection, or repair damage from exercise. An important point to understand in this process is that it is often inflammation that gives the monocytes the instructions and, thus their PhD in what to do. Once a monocyte has been given instructions on what to do by a certain tissue, they are essentially useless to any other tissue in the body.
Neutrophils are another type of white blood cell, the most numerous. Neutrophils act and move quickly to sites of inflammation to help battle invaders by engulfing them, secreting antimicrobial proteins that help digest invaders, and increasing inflammation to signal there is an infection. The function of monocytes and neutrophils is important to understanding how the principles of the Paleo diet can improve athletic performance.
The Paleo diet avoids refined sugars/processed foods, grains, legumes and dairy and replaces them with fruit and vegetables. Many people elect to eat large quantities of meat as well, but since most people eat large quantities of meat regardless of whether they eat a Paleo diet or not, we'll skim past that part(FYI, I recommend a moderate level of meat consumptions). The gluten in grains and casein in dairy are two proteins that can increase inflammation in the GI tract. An inflamed GI tract could hijack monocytes that would be better served helping you recover from exercise induced damage to muscle tissue.
In addition to tying up monocytes that could help recovery, GI inflammation also increases intestinal permeability to lipopolysaccharide(LPS). LPS drives the immune system nuts and induces insulin resistance in muscle and fat tissue to preserve glucose for the immune system. Since insulin sensitivity is the primary dictator of an athletes ability to replenish glycogen stores after training or competition, causing insulin resistance at any point in the recovery process can be bad for performance.
One final piece of the puzzle is how neutrophils respond to refined sugars. Ingestion of large amounts of refined sugars has been shown to reduce the ability of neutrophils to engulf invaders for up to 5 hours post-ingestion while starches had not effects(1). While this effect likely has a modest direct effect on exercise recovery, it will have a greater impact on susceptibility to infection which, over the long term, can negatively impact performance by taking an athlete away from training.
While many people attribute the benefits of a Paleo diet to a low carbohydrate content, most of the positive benefits of the diet occur because the quality of the diet changes. By improving the quality of your diet, you can improve athletic performance by improving recovery through better immune system function. Furthermore, if you participate in a sport that primarily relies on glucose for energy, cutting carbohydrates will have a deleterious effect on performance. My prediction for Lebron James is that he will either increase his carbohydrate intake during the season, or you will see at least a minor drop in his performance.
The world is abuzz with Lebron James' recent decision to undertake a low carbohydrate Paleo diet and the more svelte physique that followed. While the aesthetic change to his decision is readily apparent, the performance ramifications wait to be seen. As someone who has used principles of the Paleo diet for my own personal nutrition as well as those of my clients for the past 5 years, I am familiar with the ins and outs of this type of nutrition program. While paying more attention to the quality of one's diet can improve performance, cutting carbohydrates is not always the best idea for someone in a sport like basketball.
The type of fuel a person uses is dependent on the type of activity they partake in. Someone who sits at a desk and does low level physical activity throughout the day doesn't need a large amount of carbohydrate because this type of activity predominantly uses fat. If this person were to get up and sprint on and off for 30 seconds at a time they would shift to burning glucose, which is what the body turns carbohydrates in to. In the event this person decides not to eat carbohydrate and still tries to perform physical activity that requires glucose from carbohydrates, they will eventually "bonk". This means they will not be able to produce energy fast enough to keep up with demand. While they will be able to make glucose from non-carbohydrate energy sources, the body cannot produce it fast enough to keep up with the demands of a sport like basketball. My prediction: Either Lebron starts eating carbohydratess or his game will suffer.
So if slashing carbohydrates isn't going to give a performance advantage, how can following principles of the Paleo diet improve athletic performance? To better understand how this works, it's important to get a basic understanding of how the immune system works. I promise this won't get too technical. Monocytes are essentially immature white blood cells, they roam around the bloodstream like a couple of high schoolers looking for something to do. Just like a high schooler, they have no specialized skill because they haven't received instruction yet. When monocytes encounter an area of the body in need, they quickly receive a PhD in what needs to be done from the environment and differentiate in to a more specialized type of cell that can carry out a more specific task in that tissue. This could be to identify invaders, fight an infection, or repair damage from exercise. An important point to understand in this process is that it is often inflammation that gives the monocytes the instructions and, thus their PhD in what to do. Once a monocyte has been given instructions on what to do by a certain tissue, they are essentially useless to any other tissue in the body.
Neutrophils are another type of white blood cell, the most numerous. Neutrophils act and move quickly to sites of inflammation to help battle invaders by engulfing them, secreting antimicrobial proteins that help digest invaders, and increasing inflammation to signal there is an infection. The function of monocytes and neutrophils is important to understanding how the principles of the Paleo diet can improve athletic performance.
The Paleo diet avoids refined sugars/processed foods, grains, legumes and dairy and replaces them with fruit and vegetables. Many people elect to eat large quantities of meat as well, but since most people eat large quantities of meat regardless of whether they eat a Paleo diet or not, we'll skim past that part(FYI, I recommend a moderate level of meat consumptions). The gluten in grains and casein in dairy are two proteins that can increase inflammation in the GI tract. An inflamed GI tract could hijack monocytes that would be better served helping you recover from exercise induced damage to muscle tissue.
In addition to tying up monocytes that could help recovery, GI inflammation also increases intestinal permeability to lipopolysaccharide(LPS). LPS drives the immune system nuts and induces insulin resistance in muscle and fat tissue to preserve glucose for the immune system. Since insulin sensitivity is the primary dictator of an athletes ability to replenish glycogen stores after training or competition, causing insulin resistance at any point in the recovery process can be bad for performance.
One final piece of the puzzle is how neutrophils respond to refined sugars. Ingestion of large amounts of refined sugars has been shown to reduce the ability of neutrophils to engulf invaders for up to 5 hours post-ingestion while starches had not effects(1). While this effect likely has a modest direct effect on exercise recovery, it will have a greater impact on susceptibility to infection which, over the long term, can negatively impact performance by taking an athlete away from training.
While many people attribute the benefits of a Paleo diet to a low carbohydrate content, most of the positive benefits of the diet occur because the quality of the diet changes. By improving the quality of your diet, you can improve athletic performance by improving recovery through better immune system function. Furthermore, if you participate in a sport that primarily relies on glucose for energy, cutting carbohydrates will have a deleterious effect on performance. My prediction for Lebron James is that he will either increase his carbohydrate intake during the season, or you will see at least a minor drop in his performance.
Thursday, September 4, 2014
Would you take that drug if you knew the whole story? Context matters.
Let's say you've gone to your doctor for your annual check-up. The Dr. comes in and tells you that he sees something in your bloodwork that is troubling to him, and he'd like to put you on a drug. At this point the vast majority of people will just take the drug, but a few may question the Dr. more, as they should. Let's just assume you are one of those people, and the conversation carries on.
"Well, I'm a little concerned about your bloodwork. You have an elevated risk for cardiovascular disease, I'd like to put you on one of 2 drugs. The first one will reduce your future risk of death from cardiovascular disease by 30%, and the second will only prevent death for 1 out of 30 people."
As the shock sets in, you begin to think about the prospects of having to take a drug for the rest of your life. Of course, cardiovascular disease has always been on your mind. Your father had a heart attack at 55. You've done your best to get regular exercise and eat a healthy diet, and at 45 years of age feel 10 years younger. Despite feeling well and never having had a heart attack, you decide it's likely in your best interest to take a drug.
Which drug would you take? Assuming that you are generally good at math, most people would choose the first one. The problem is, the first and the second drug are the same drug. Of course clinical research studies often have different outcomes depending on how they are designed, but this data is not only for the same drug it's from the same study, I just worded the outcome differently(1). This illustrates an important point; when research results are worded in a way that inflates the results, people are more likely to take a drug.
When you look at the "30% decreased risk", that is something termed relative risk. This is used often despite the fact that it presents the data in a deceptive way that makes you more likely to take the drug. Let's say you perform a study with 100 people in the treatment group and 100 people in the placebo group. Of the people who received the treatment only 1 person died, while in the group not receiving the treatment 2 people died. This would seem to be a very small effect since the absolute difference is only 1. However, stated in relative risk terms, the treatment reduced the risk of death by 50%. This is where numbers like the number needed to treat(NNT) come in handy. In this fake study, the NNT is 100. In other words, you need to treat 100 people with the drug to prevent one death, the other 99 who are taking it will not live any longer with or without the drug. Yay!
This is problematic for many reasons, not the least of which being that most pharmaceutical drugs have a laundry list of side effects that could affect the 29 out of 30 people not experiencing a benefit from the drug. For statins, this means an increased risk of neurological problems, muscle pain, an increased risk for Type 2 diabetes, liver damage, and more. Another reason this is problematic is that they have recently revised the guidelines for prescribing statin drugs which would increase the number of people eligible to take the drugs to 56 million. This would potentially prevent 1.87 million deaths over the course of 5-6 years, while 54.13 million would be taking the drug with no benefit from a mortality standpoint. The interesting part is that these numbers are for people who have had a previous heart attack, if you've never had a heart attack, the picture is worse.
For primary prevention, the NNT is a lot worse. Primary prevention essentially means using statins to prevent a heart attack or stroke in someone who has never had one before. The NNT in these people is 1 in 60 to prevent a heart attack and 1 in 268 to prevent a stroke. Side effects, on the other hand were seen in 1 in 50 people(Type 2 diabetes) or 1 in 10(muscle damage)(2). The NNT to prevent 1 death from cardiovascular disease in primary prevention trials fluctuates but is typically around 1 in 120. Taken together, this means that in 600 people you would prevent 10 heart attacks and prevent 5 deaths, while creating 12 new cases of diabetes, which increases your risk for a heart attack. In fact, people with Type 2 diabetes have the same risk of experiencing a heart attack as someone who has had a heart attack before and are twice as likely to die from a heart attack than non-diabetics(3). So, of the 600 people who took the drug, 10 will prevent a heart attack and 12 will substantially increase their risk for one. Does that sound like something you would sign up for?
When you look at the data this way, it makes the decision on whether or not to take something like a statin a lot more difficult. I can't tell a person whether or not they should take a drug, that's between that person and their doctor. Looking at the total picture from a numbers standpoint makes the decision a lot more difficult than, "You're the DR, whatever you say". On top of the numbers issue, they are finding new therapeutic effects from these drugs every day and so many of the results conflict with one another. Recent evidence has shown that statins may be protective against cancer when taken for 4 years(4), but they may also double a woman's risk of breast cancer when taken for over 10 years(5).
While many of the researchers who come to positive findings on these drugs hail them, one has to wonder how they know the drugs are totally safe when they are finding new ways to use them every day. If you are looking for therapeutic uses for a drug and are just now finding new ones, how can you get a complete handle on the total range of side effects when they are more of an afterthought and may not pop up until 10 years down the road? The point of this is not to prevent you from taking pharmaceutical drugs, the point is that you should ask more questions, research these drugs, and weigh the pros and cons before you decide that's the route you're going to take. Just for the sake of comparison, 300 minutes of exercise per week for the use of primary prevention of heart disease can reduce your risk by 20%(6) and regular exercise for secondary prevention can reduce the risk of death from heart disease by 27%(7).
"Well, I'm a little concerned about your bloodwork. You have an elevated risk for cardiovascular disease, I'd like to put you on one of 2 drugs. The first one will reduce your future risk of death from cardiovascular disease by 30%, and the second will only prevent death for 1 out of 30 people."
As the shock sets in, you begin to think about the prospects of having to take a drug for the rest of your life. Of course, cardiovascular disease has always been on your mind. Your father had a heart attack at 55. You've done your best to get regular exercise and eat a healthy diet, and at 45 years of age feel 10 years younger. Despite feeling well and never having had a heart attack, you decide it's likely in your best interest to take a drug.
Which drug would you take? Assuming that you are generally good at math, most people would choose the first one. The problem is, the first and the second drug are the same drug. Of course clinical research studies often have different outcomes depending on how they are designed, but this data is not only for the same drug it's from the same study, I just worded the outcome differently(1). This illustrates an important point; when research results are worded in a way that inflates the results, people are more likely to take a drug.
When you look at the "30% decreased risk", that is something termed relative risk. This is used often despite the fact that it presents the data in a deceptive way that makes you more likely to take the drug. Let's say you perform a study with 100 people in the treatment group and 100 people in the placebo group. Of the people who received the treatment only 1 person died, while in the group not receiving the treatment 2 people died. This would seem to be a very small effect since the absolute difference is only 1. However, stated in relative risk terms, the treatment reduced the risk of death by 50%. This is where numbers like the number needed to treat(NNT) come in handy. In this fake study, the NNT is 100. In other words, you need to treat 100 people with the drug to prevent one death, the other 99 who are taking it will not live any longer with or without the drug. Yay!
This is problematic for many reasons, not the least of which being that most pharmaceutical drugs have a laundry list of side effects that could affect the 29 out of 30 people not experiencing a benefit from the drug. For statins, this means an increased risk of neurological problems, muscle pain, an increased risk for Type 2 diabetes, liver damage, and more. Another reason this is problematic is that they have recently revised the guidelines for prescribing statin drugs which would increase the number of people eligible to take the drugs to 56 million. This would potentially prevent 1.87 million deaths over the course of 5-6 years, while 54.13 million would be taking the drug with no benefit from a mortality standpoint. The interesting part is that these numbers are for people who have had a previous heart attack, if you've never had a heart attack, the picture is worse.
For primary prevention, the NNT is a lot worse. Primary prevention essentially means using statins to prevent a heart attack or stroke in someone who has never had one before. The NNT in these people is 1 in 60 to prevent a heart attack and 1 in 268 to prevent a stroke. Side effects, on the other hand were seen in 1 in 50 people(Type 2 diabetes) or 1 in 10(muscle damage)(2). The NNT to prevent 1 death from cardiovascular disease in primary prevention trials fluctuates but is typically around 1 in 120. Taken together, this means that in 600 people you would prevent 10 heart attacks and prevent 5 deaths, while creating 12 new cases of diabetes, which increases your risk for a heart attack. In fact, people with Type 2 diabetes have the same risk of experiencing a heart attack as someone who has had a heart attack before and are twice as likely to die from a heart attack than non-diabetics(3). So, of the 600 people who took the drug, 10 will prevent a heart attack and 12 will substantially increase their risk for one. Does that sound like something you would sign up for?
When you look at the data this way, it makes the decision on whether or not to take something like a statin a lot more difficult. I can't tell a person whether or not they should take a drug, that's between that person and their doctor. Looking at the total picture from a numbers standpoint makes the decision a lot more difficult than, "You're the DR, whatever you say". On top of the numbers issue, they are finding new therapeutic effects from these drugs every day and so many of the results conflict with one another. Recent evidence has shown that statins may be protective against cancer when taken for 4 years(4), but they may also double a woman's risk of breast cancer when taken for over 10 years(5).
While many of the researchers who come to positive findings on these drugs hail them, one has to wonder how they know the drugs are totally safe when they are finding new ways to use them every day. If you are looking for therapeutic uses for a drug and are just now finding new ones, how can you get a complete handle on the total range of side effects when they are more of an afterthought and may not pop up until 10 years down the road? The point of this is not to prevent you from taking pharmaceutical drugs, the point is that you should ask more questions, research these drugs, and weigh the pros and cons before you decide that's the route you're going to take. Just for the sake of comparison, 300 minutes of exercise per week for the use of primary prevention of heart disease can reduce your risk by 20%(6) and regular exercise for secondary prevention can reduce the risk of death from heart disease by 27%(7).
Monday, August 25, 2014
Does the Paleo diet cure X?
http://www.examiner.com/article/jack-osbourne-high-fat-low-carb-ketogenic-paleo-diet-helps-multiple-sclerosis
The link above is one of many anecdotal pieces of evidence that has shown significant health improvements from a Paleo diet. The health conditions that are purportedly improved by a Paleo diet range from inflammatory conditions such as Rheumatoid Arthritis, digestive problems such as Irritable Bowel Syndrome, neurological problems such as Multiple Sclerosis, and the number one killer in the United States: heart disease. Are these pieces of evidence enough to state that the Paleo diet cures any of these conditions? Absolutely not, we are eons away from a scientific consensus on what causes these problems, let alone what we can do to fix them. Does this mean that the Paleo diet isn't the answer? Nope.
Science is a wonderful thing, but not a necessity for something to be true. Science is the process we use to come to a consensus on a topic such as this because it eliminates all alternative explanations. Truths aren't made by science, they are identified with it. It very well could be the case that many of our modern ills are directly attributable to the lifestyle we live. Many of the problems that have plagued human civilization throughout history can be directly attributed to things we have determined to be "progress". The formation of cities and towns is certainly progress, but that doesn't mean that communicable disease and the rapid spread of infection isn't a product of that progress. As Lord Helmet told us many years ago, there is an up side and a down side to every Schwartz.

This is where the evolutionary approach to health enters the picture. You've got X, will the Paleo diet help? help maybe, but cure? No. Why? The evolutionary approach to medicine isn't a diet. There are many aspects of today's life that are quite novel to modern humans. Never having to go hungry, never having to experience extremes in temperature, being able to sit on your butt all day long and still procure ample food, not having to succumb to bacterial infections due to antibiotics, and the onslaught of chronic stress we experience today. The current food environment is certainly a drastic shift to our species, but it is one of many issues that may not jibe with our genetic code.
When you look at the epidemiological research, it is universally accepted that things like poor sleep, a diet high in processed food and calories, high levels of stress, long periods of inactivity, and infrequent intense physical activity are all aspects of modern life that are problematic to health. When you look at modern day hunter gatherers who live a lifestyle that completely eliminates these traits, we see insignificant levels of the diseases that plague us such as Cardiovascular disease, Type 2 diabetes, Cancer, and even Depression. Multiple studies are coming out showing what many of these poor lifestyle traits do to us at a genetic level, strengthening support that many of our issues are caused by our current lifestyle. From a scientific perspective, this doesn't prove anything. Besides, let's say being born by C-section or having to take a dose of antibiotics to kill a bacterial infection do have some ramifications, is the alternative, aka death, a better prognosis than later obesity or IBS? Probably not, but knowing how to take steps to prevent or reduce the potential symptoms from those potential outcomes likely lies within the evolutionary approach to health.
Many people can benefit from this information, and waiting for a scientific consensus is not going to benefit most people in this lifetime because it won't likely come in that time period. Even if the scientific consensus comes, it won't show that the Paleo diet or an evolutionary approach to health cures these problems. What it will show is that many of our current health problems may be caused by a modern lifestyle, but that doesn't mean doing some diet for 3 months will allow you to go back to business as usual.
The link above is one of many anecdotal pieces of evidence that has shown significant health improvements from a Paleo diet. The health conditions that are purportedly improved by a Paleo diet range from inflammatory conditions such as Rheumatoid Arthritis, digestive problems such as Irritable Bowel Syndrome, neurological problems such as Multiple Sclerosis, and the number one killer in the United States: heart disease. Are these pieces of evidence enough to state that the Paleo diet cures any of these conditions? Absolutely not, we are eons away from a scientific consensus on what causes these problems, let alone what we can do to fix them. Does this mean that the Paleo diet isn't the answer? Nope.
Science is a wonderful thing, but not a necessity for something to be true. Science is the process we use to come to a consensus on a topic such as this because it eliminates all alternative explanations. Truths aren't made by science, they are identified with it. It very well could be the case that many of our modern ills are directly attributable to the lifestyle we live. Many of the problems that have plagued human civilization throughout history can be directly attributed to things we have determined to be "progress". The formation of cities and towns is certainly progress, but that doesn't mean that communicable disease and the rapid spread of infection isn't a product of that progress. As Lord Helmet told us many years ago, there is an up side and a down side to every Schwartz.

This is where the evolutionary approach to health enters the picture. You've got X, will the Paleo diet help? help maybe, but cure? No. Why? The evolutionary approach to medicine isn't a diet. There are many aspects of today's life that are quite novel to modern humans. Never having to go hungry, never having to experience extremes in temperature, being able to sit on your butt all day long and still procure ample food, not having to succumb to bacterial infections due to antibiotics, and the onslaught of chronic stress we experience today. The current food environment is certainly a drastic shift to our species, but it is one of many issues that may not jibe with our genetic code.
When you look at the epidemiological research, it is universally accepted that things like poor sleep, a diet high in processed food and calories, high levels of stress, long periods of inactivity, and infrequent intense physical activity are all aspects of modern life that are problematic to health. When you look at modern day hunter gatherers who live a lifestyle that completely eliminates these traits, we see insignificant levels of the diseases that plague us such as Cardiovascular disease, Type 2 diabetes, Cancer, and even Depression. Multiple studies are coming out showing what many of these poor lifestyle traits do to us at a genetic level, strengthening support that many of our issues are caused by our current lifestyle. From a scientific perspective, this doesn't prove anything. Besides, let's say being born by C-section or having to take a dose of antibiotics to kill a bacterial infection do have some ramifications, is the alternative, aka death, a better prognosis than later obesity or IBS? Probably not, but knowing how to take steps to prevent or reduce the potential symptoms from those potential outcomes likely lies within the evolutionary approach to health.
Many people can benefit from this information, and waiting for a scientific consensus is not going to benefit most people in this lifetime because it won't likely come in that time period. Even if the scientific consensus comes, it won't show that the Paleo diet or an evolutionary approach to health cures these problems. What it will show is that many of our current health problems may be caused by a modern lifestyle, but that doesn't mean doing some diet for 3 months will allow you to go back to business as usual.
Labels:
Paleo
Subscribe to:
Posts (Atom)

.JPG)
.JPG)
.JPG)
.JPG)
